Selecting a hearing care provider is an important decision. Why? Because finding the most qualified and dependable professional can mean the difference between being successful and satisfied with your hearing aids…or not.
No doubt, you choose other health care professionals—your general practitioner, ophthalmologist, cardiologist, podiatrist, just to name a few—very carefully. Your hearing care professional is no different. Perhaps what makes the process most challenging are the many choices—from types of care providers to brands, levels and styles of hearing technology. Information can be confusing, even contradictory. Being educated about modern hearing healthcare and hearing aids allows you to make the most informed decision for your best outcome.
Here’s what you need to know about the two kinds of professionals—audiologists and hearing instrument specialists—who are licensed to sell and fit hearing aids in the states Johnson Audiology serves—Tennessee and Georgia.
TWO TYPES OF HEARING CARE PROVIDERS: VERY DIFFERENT CREDENTIALS
An Audiologist’s credentials
Audiologists complete extensive university coursework to receive a clinical doctor-ate in audiology, earning their bachelor’s, master’s, and doctorate degrees over the course of eight years.
Through extensive graduate level coursework, what do they learn:
- The neural pathways for transmission of sound from the inner ear to the cortex of the brain
- Diagnostic testing for hearing loss, tinnitus, hyperacusis and other hearing-related disorders
- The circuitry and components of a hearing aid and how to choose brand, style, and fit tailored to the individual patient
- Assistive technology devices and how those can dovetail with a patient’s hearing aids and elevate the hearing experience
- Theories of tinnitus and sound perception
- Ear and hearing dysfunction and appropriate treatment options
- Hearing conservation programs
- Acoustic and digital modification strategies for hearing instruments
- Inner ear balance disorders
- Counseling techniques for patients and their family members regarding hearing loss and intervention.
- How to cultivate critical thinking skills and lifelong learning related to hearing function, amplification strategies, and tinnitus management
- How to concentrate on superior patient care with compassionate counseling
Throughout their graduate-level study, Audiologists are supervised in clinical rotations for all age levels in the following settings:
- University clinic
- Hospital
- Public school system
- Otolaryngology/ENT practices
- Veteran’s Administration
- Private practice
During each semester of the four-year graduate school enrollment, a student will:
- Participate in 12 hours of coursework in addition to six hours of clinical work with patients
- Routinely participate in clinical work with aural rehabilitation therapy to gain a better understanding of the work performed by their speech-language pathology colleagues
- Log nearly 2,000 patient contact hours during their fourth year of graduate study, in addition to their previous hours acquired during their first three years of graduate study
Applicants for licensure as an Audiologist in Tennessee must:
- Earn a doctoral degree with an emphasis in audiology from an accredited institution
- Have a current certificate of clinical competence (CCC-A) from American Speech-Language Hearing Association (ASHA) and/or complete 1,820 clock hours of supervised clinical practicum by a licensed or certified audiologist and pass the Praxis exam for audiology.
- Complete ten hours of continuing education every year to maintain their license.
A hearing Instrument specialist’s training
A dispenser/hearing instrument specialist (HIS) is the second professional permitted to sell and issue hearing aids in Tennessee and Georgia.
For initial apprentice licensure, an HIS must:
- Be at least 18 years old
- Have two years of college coursework in any subject (does not have to be in audiology or a related subject)
- Pass a written exam
Upon apprenticeship completion, an HIS must:
- function under the direct supervision of a sponsoring, licensed hearing instrument specialist (HIS) for at least three months
- Complete 60 hours of classroom coursework
A HIS must:
- Complete 20 hours of continuing education during the two calendar years that precede the licensure renewal year with two hours of the 20-hour requirement pertaining to state statutes and rules concerning hearing instrument specialists.
As you consider who you want to trust as your lifelong partner on your journey to healthier hearing. ask yourself these questions:
- Which hearing provider—an Audiologist or a HIS—has the highest level of education?
- Which provider has shown the greatest evidence of commitment to his or her field through time and personal resources invested in honing knowledge and skills?
- Which provider spends the most time working with patients in a supervised, training setting before being credentialed to work with those with hearing loss solo?
- Which type of provider routinely verifies and files your insurance benefits for hearing health care?
- Which provider conducts a full diagnostic hearing test in a rated, sound-proof booth?
Misconceptions and Facts
Misconception
- An Audiologist’s education concentrates on the diagnostic procedures rather than hearing aid fitting.
Fact
- Audiologists formally study hearing aid technologies from multiple manufacturers while in graduate school and continue to do so throughout their careers. Notably, most of the professionals from the hearing aid manufacturers that lead trainings are degreed audiologists not hearing instrument specialists.
Misconception
- Hearing instrument specialists offer the same type of hearing tests as an audiologist
Fact
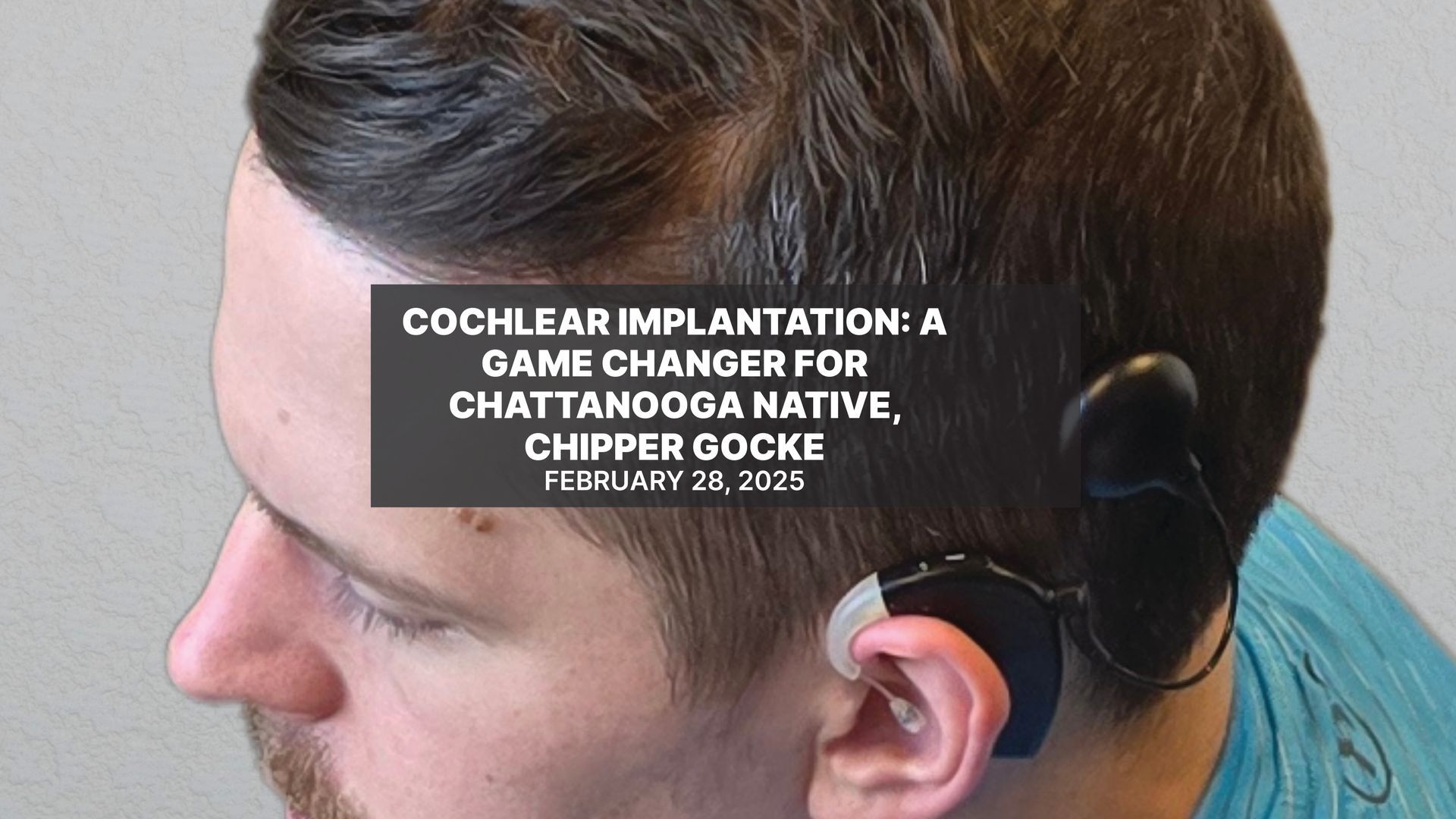
- Hearing instrument specialists are not licensed to perform audiological exams. Therefore, their assessments are not considered diagnostic hearing tests but rather basic hearing screenings. Audiologists, however, do full audiologic testing in a rated, sound-proof booth. Audiologists are also trained and licensed to conduct diagnostic testing specifically for those with tinnitus and for patients who are candidates for cochlear implantation, testing which hearing instruments specialists cannot legally perform.
Misconception
- Hearing instrument specialists offer free hearing tests because they care more about their customers
Fact
- Most audiologists offer patients the benefit and convenience of filing the patient’s diagnostic hearing test to Medicare, which covers testing. Notably, it is insurance fraud for an Audiologist to bill Medicare for one patient and then provide a free evaluation for another patient. Therefore, audiologists cannot legally provide free hearing testing if they are a Medicare provider. Since most hearing dispensers offer “free” testing this automatically means they are not working with Medicare so customers lose out on that benefit.
Here are some tips when searching for your hearing care professional:
- Ask for the provider’s credentials. A doctor of audiology has the credentials Au.D. following his or her name. If you see HIS following the person’s name, you know that person is a minimally trained hearing instrument specialist.
- Look for an Audiologist who works with several hearing aid manufacturers so that your technology can be tailored to your unique hearing loss.
- Ask if you are entitled to a trial period. Each patient is a unique individual. You deserve to work with a professional who spends times assessing and addressing your personal hearing concerns, goals, desires and budget.
- Do not buy hearing aids by mail or internet that claim patients do not need direct contact with their hearing health-care professional.